When your kidneys start to fail, your body doesn’t just slow down-it starts to poison itself. You might not feel like you’re sick. No fever. No cough. But then, out of nowhere, you can’t eat. Your skin burns. You scratch until it bleeds. And no matter how much water you drink, you still feel swollen, tired, and nauseous. This isn’t just bad luck. This is uremia.
What Exactly Is Uremia?
Uremia isn’t a disease. It’s the result of your kidneys giving up. When they can’t filter waste anymore, toxins like urea, creatinine, and p-cresyl sulfate build up in your blood. These aren’t just numbers on a lab report-they’re chemicals that wreck your brain, your skin, your stomach, and your sleep. The term comes from “urine,” because doctors first noticed these symptoms in people who stopped making urine. Today, we know it’s not about volume-it’s about quality. Your blood is turning toxic.By the time symptoms show up, your kidney function is already below 15%. That’s stage 5 chronic kidney disease, or end-stage kidney disease. About 89% of people who start dialysis already have these symptoms. And if you’re one of them, waiting too long to act can cost you your life.
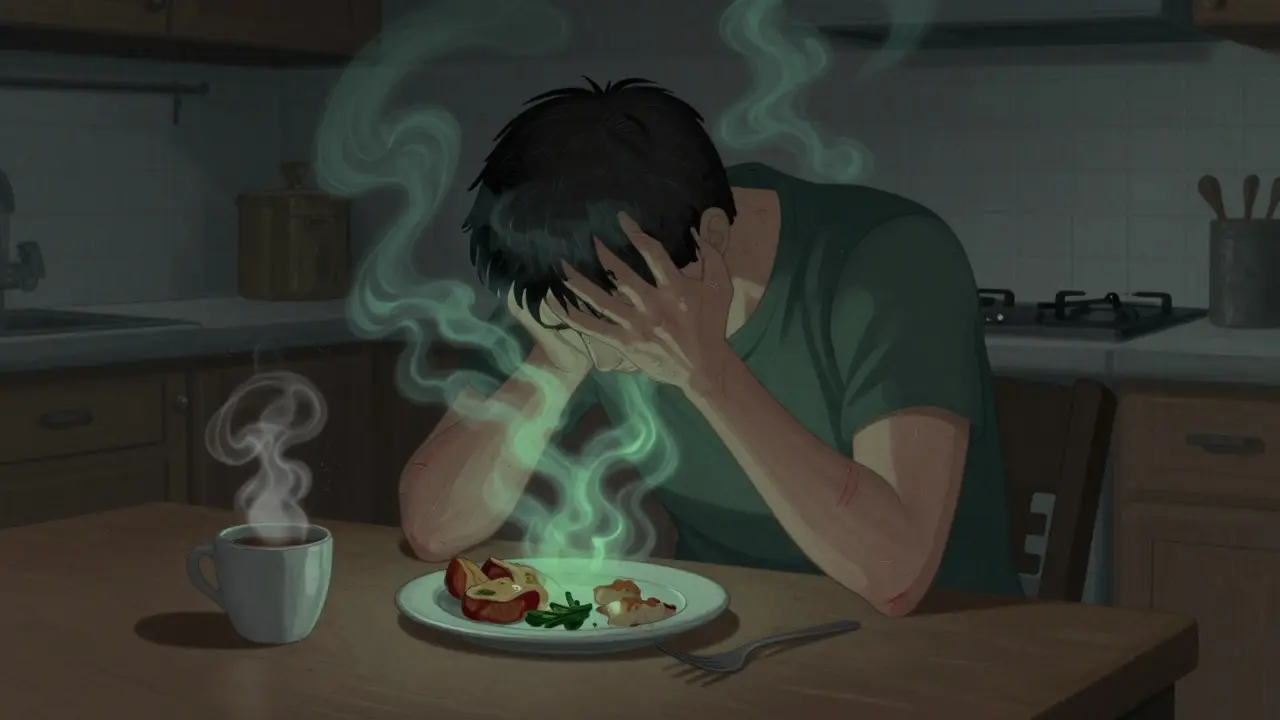
Why You Can’t Eat: The Nausea That Doesn’t Go Away
Imagine waking up and the smell of coffee makes you want to throw up. Or eating a piece of toast feels like swallowing sand. That’s not just a bad stomach. That’s uremic nausea.It hits hard and early. Studies show 68% of people with stage 5 CKD experience it. The trigger? Urea levels above 80 mg/dL. But it’s not just urea. Two other toxins-indoxyl sulfate and p-cresyl sulfate-stick to your brain’s nausea center. They’re like little alarms screaming at your body: “Something’s wrong.”
And it’s not just discomfort. This nausea leads to weight loss. One patient lost 18 pounds in two months because food tasted like metal. Another dropped 5% of their body weight in three months-enough for doctors to flag it as a medical emergency. Your body starts eating itself. Muscle disappears. Strength fades. You can’t work. You can’t care for your kids. You just lie there, too sick to move.
Doctors treat this with ondansetron or domperidone. But here’s the catch: if you’re still nauseous after a week of meds, dialysis is the only real fix. Medications just buy you time. They don’t remove the poison.
The Itch That Won’t Stop: Uremic Pruritus
If nausea is the silent killer, itching is the scream. Uremic pruritus-also called CKD-associated pruritus-is one of the most underreported, misunderstood symptoms in kidney disease.It’s not dry skin. It’s not allergies. It’s not eczema. It’s your blood poisoning your nerves. A 2022 study found 68.9% of hemodialysis patients have it. Even worse, 37.3% of people still not on dialysis already feel it. And it’s not random. It hits the same spots: back, arms, legs-bilateral, symmetric, no rash. And it gets worse at night. That’s when most patients say they can’t sleep.
Doctors measure it with the 5-D Itch Scale: Duration, Degree, Direction, Disability, Distribution. A score over 12 means severe. Over 15? That’s a red flag. One patient on Reddit said they scratched until they bled. Their Fitbit sleep score dropped from 85 to 42. That’s not exaggeration. That’s reality.
Why does it happen? Inflammation. People with severe itching have CRP levels nearly three times higher than those without it. That’s a sign your body is in constant fight mode. It’s not just your skin-it’s your whole system screaming.
First-line treatment? Optimize dialysis. If you’re on dialysis and still itching, your sessions might not be long or frequent enough. Then come gabapentin or pregabalin. But the real game-changer? Difelikefalin. Approved by the FDA in 2021, it’s the first drug made specifically for this. It cuts itch by over 30% in days. Nalfurafine, another option, lets people sleep through the night for the first time in years.

When Should You Start Dialysis?
This is the question everyone asks. And the answer used to be simple: wait until you’re dying. But that’s not true anymore.The old rule? Start dialysis when eGFR hits 5 or 6. But the 2020 IDEAL trial changed everything. It found no survival benefit to starting early-at eGFR 10-14-versus late-at 5-7. But here’s the twist: people who waited and managed symptoms well had better quality of life. They were less depressed. Less hospitalized. More able to work.
So now, the decision isn’t about numbers. It’s about suffering. The 2023 KDOQI guidelines say: start dialysis when symptoms become unmanageable. That means:
- Nausea that causes 5% weight loss in 3 months
- Itching so bad you can’t sleep or work (5-D score >15)
- Fluid overload you can’t control with pills
- Pericarditis (fluid around the heart) confirmed by ultrasound
- Confusion, seizures, or bleeding from uremic toxins
Some doctors still push for early dialysis. Others say: hold off. But the consensus? If you’re suffering, you’re ready. Your eGFR is just a number. Your quality of life is the real metric.
What Happens If You Wait Too Long?
Delaying dialysis isn’t brave. It’s dangerous.One study found patients who waited until they were vomiting constantly, barely able to walk, and covered in scratches had 58% higher death rates than those who started when symptoms first became hard to control. That’s not a small difference. That’s life or death.
And it’s not just about dying. It’s about surviving in misery. People who delay dialysis end up in the ER more often. They spend more days in the hospital. They’re more likely to need emergency dialysis-where they’re hooked up while unconscious, scared, and in pain.
And then there’s the cost. People with severe itching spend $8,432 more per year on healthcare. Why? More ER visits. More skin infections. More sleep meds. More depression therapy. The system pays for it. But you pay in sleepless nights, broken relationships, and lost jobs.

Why Diagnosis Takes So Long
Here’s the cruel part: most people don’t know what they’re feeling is kidney failure.A 2022 survey found 41% of patients visited three or more doctors before someone said, “It’s your kidneys.” Nausea? “Stomach flu.” Itching? “Dry skin.” Fatigue? “You’re just stressed.”
It takes an average of 8.7 months from first symptom to diagnosis. That’s over half a year of suffering while your kidneys keep failing. By then, you’re already in crisis.
Why? Because kidney disease is silent. No pain. No red flag. Just slow, creeping decay. And doctors aren’t trained to look for it unless you’re diabetic or hypertensive.
That’s why if you have CKD-even stage 3 or 4-and you start feeling nauseous or itchy, don’t wait. Ask for a BUN, creatinine, and eGFR test. Don’t assume it’s something else. Your kidneys are telling you they’re done.
What’s Changing in Kidney Care
The future of dialysis isn’t just about blood filters. It’s about listening.Next year, KDIGO (the global kidney guidelines group) will likely update its rules to include patient-reported symptoms as a trigger for dialysis-not just eGFR. That’s huge. It means your voice matters.
New drugs are coming. Nemifitide, a new itch blocker, showed 45% better results than placebo in trials. And research into non-opioid pain relief is growing fast, because gabapentin is often overused and risky in kidney patients.
But the biggest problem? Inequality. Black patients wait 3.2 months longer than white patients to start dialysis. That’s not about access to care. That’s about bias. About assumptions. About who gets heard.
That’s why if you’re feeling these symptoms, you need to speak up. Keep a journal. Track your itching. Note your weight. Write down when you can’t eat. Bring it to your nephrologist. Don’t let them dismiss you.
Final Thought: Your Body Is Trying to Tell You Something
Nausea. Itch. Fatigue. Loss of appetite. These aren’t just annoyances. They’re alarms. Loud, desperate alarms.Dialysis isn’t a punishment. It’s a rescue. It’s not about living forever. It’s about living well-sleeping through the night, eating without gagging, holding your grandchild without itching your skin raw.
Don’t wait for collapse. Don’t wait for a crisis. If your symptoms are starting to control your life, it’s time to talk to your doctor. Not next week. Not after the holidays. Now.
Your kidneys can’t fix themselves. But dialysis can. And sometimes, that’s enough to get your life back.

Mike Rengifo
December 17, 2025 AT 20:42Man, I never realized how silent kidney failure is until I read this. My uncle went from 'just tired' to ER in three days. No warning. Just... gone. And the itching? He'd scratch his arms raw at 3 a.m. and still say he was 'fine.' We didn't know it was his kidneys until it was too late.
Ashley Bliss
December 19, 2025 AT 04:48Let me be clear: if you're waiting for a number to tell you you're dying, you've already lost the war. This isn't medicine-it's moral failure. Doctors treat labs, not people. And people? People suffer in silence while bureaucrats debate eGFR thresholds like they're negotiating a car lease. You think dialysis is the punishment? No. The punishment is letting someone suffer for months while they're still alive enough to beg for help.
bhushan telavane
December 19, 2025 AT 23:10India has same problem. Many people think kidney issue = only diabetes or high BP. My cousin had itching for 10 months. Went to 4 doctors. One said 'use moisturizer.' Another said 'stress.' Finally, a young resident asked: 'Have you ever checked creatinine?' Turned out eGFR was 4. He started dialysis next week. Now he's back to teaching kids. Don't wait. Ask for test.
Mahammad Muradov
December 21, 2025 AT 08:06Actually, the IDEAL trial has significant limitations. The sample was skewed toward higher socioeconomic status patients with better access to nutrition and symptom management. The 58% higher mortality rate in delayed dialysis group? That’s not just about timing-it’s about systemic neglect. You can't equate 'quality of life' with 'survival' when your body is literally poisoning itself. This isn't philosophy-it's biochemistry.
Connie Zehner
December 22, 2025 AT 00:57OMG I FEEL THIS SO HARD. I had a friend who had the itching and she said it felt like ants crawling under her skin 24/7. She stopped hugging people because she was scared she’d scratch them. She cried every night. I told her to push harder with her doctor and she finally got difelikefalin and now she sleeps. Like, ACTUALLY sleeps. 😭🙏
mark shortus
December 23, 2025 AT 19:50Okay but-hold up. Let’s talk about the language here. 'Your blood is turning toxic.' That’s not just medically accurate-it’s poetic. And the part about urea being an alarm? That’s not metaphor. That’s biology screaming. And yet, we treat this like a minor inconvenience? Like a bad stomach bug? No. This is your body’s last voicemail before the line goes dead. And we’re deleting it without listening.
Elaine Douglass
December 25, 2025 AT 17:34I’m a nurse and I see this all the time. People come in with 5-D scores of 18 and say 'it’s just dry skin.' I wish I had a dollar for every time someone said 'I thought it was menopause' or 'I’m just getting old.' You’re not old-you’re poisoned. And you deserve to feel better. Please don’t wait.
Vicki Belcher
December 26, 2025 AT 19:57Thank you for writing this. 🙏 My mom started dialysis last month after 8 months of 'just being tired.' She can eat again. She hugged me last night. She slept through the night. I cried. This isn’t just medical advice-it’s a lifeline. If you’re reading this and you’re feeling off? Don’t wait. Don’t be polite. Demand the test. You’re worth it. 💙
anthony funes gomez
December 26, 2025 AT 21:21Uremia: a biochemical cascade of endogenous toxin accumulation-urea, creatinine, p-cresyl sulfate-disrupting CNS GABAergic signaling, inducing pruritus via kappa-opioid receptor dysregulation, and suppressing appetite via hypothalamic leptin resistance. The clinical paradigm must shift from eGFR-centric to symptom-driven intervention. Dialysis isn't a treatment-it's a homeostatic restoration mechanism. The delay isn't 'brave'-it's a failure of medical education, institutional inertia, and systemic bias. We must prioritize patient-reported outcomes as primary endpoints. Not because it's compassionate-but because it's scientifically valid.