Pregnancy Liver Failure Diagnostic Checklist
Diagnostic Criteria Assessment
This tool helps clinicians quickly assess if pregnancy-related liver failure meets diagnostic criteria based on the article's guidance.
Diagnostic Assessment
Key Takeaways
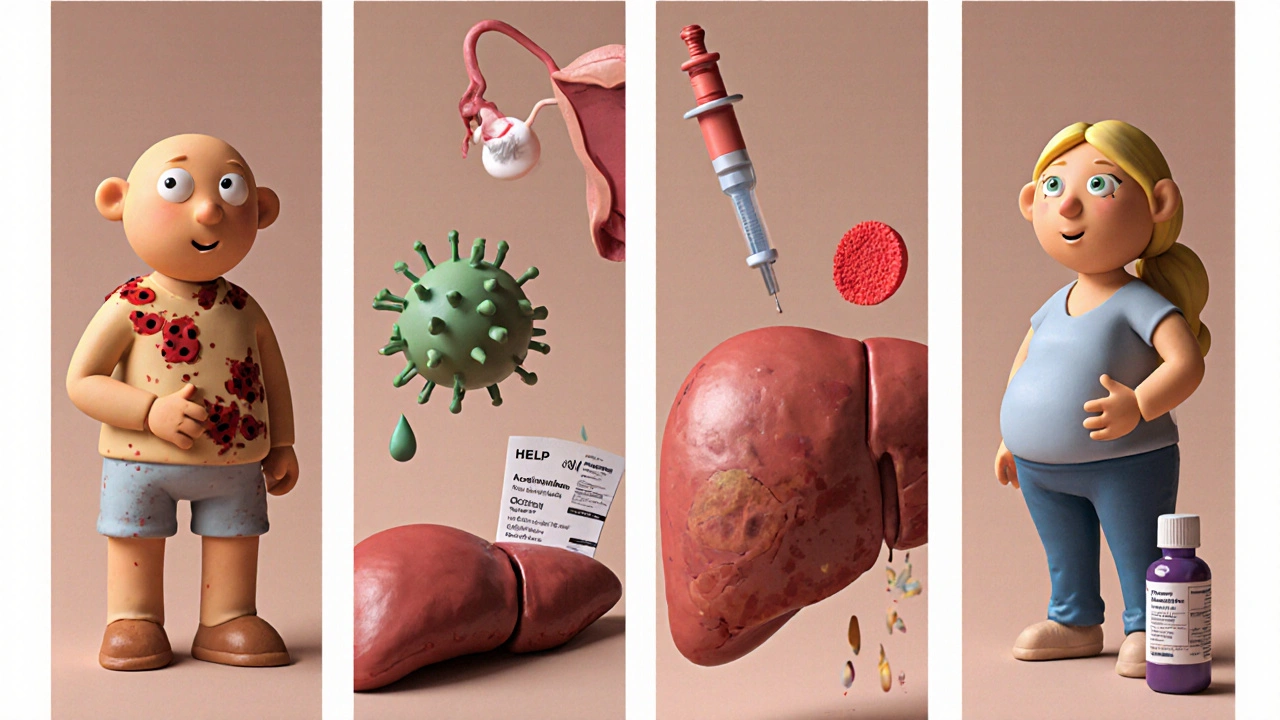
- Acute liver failure during pregnancy is rare but can be fatal for mother and baby.
- Most cases stem from HELLP syndrome, acute fatty liver of pregnancy, viral hepatitis or drug‑induced injury.
- Early recognition relies on sudden jaundice, coagulopathy, encephalopathy, and specific lab patterns.
- Prompt delivery, intensive‑care support, and condition‑specific therapy dramatically improve survival.
- A clear management checklist helps obstetric and hepatology teams act quickly.
When a pregnant woman experiences Liver Failure in Pregnancy refers to the rapid loss of liver function occurring during gestation, often classified as acute liver failure and requiring urgent medical intervention, the stakes are incredibly high. Understanding liver failure pregnancy helps protect both mother and baby.
What Exactly Is Liver Failure in Pregnancy?
In medical terms, Acute Liver Failure is the abrupt loss of hepatic synthetic, detoxifying and metabolic abilities, usually within days, leading to encephalopathy and coagulopathy is the umbrella term. When this abrupt decline occurs while a woman is pregnant, clinicians use the phrase “liver failure in pregnancy.” The condition is defined by three core criteria:
- Elevated serum bilirubin (usually >2 mg/dL) with jaundice.
- Coagulopathy - a prothrombin time (PT) >1.5 times normal or INR >1.5.
- Any grade of hepatic encephalopathy not explained by another cause.
Unlike chronic liver disease, this condition unfolds over hours to a few days, demanding immediate action.
Major Causes to Watch For
Only a handful of disorders account for the majority of cases. Below is a quick snapshot:
| Cause | Typical Onset (Weeks GA) | Key Lab Clues | First‑Line Treatment |
|---|---|---|---|
| HELLP Syndrome | 28‑36 | Elevated LDH, AST/ALT >2× ULN, platelet <100 × 10⁹/L | Stabilize, administer steroids, expedite delivery |
| Acute Fatty Liver of Pregnancy (AFLP) | 30‑38 | Hypoglycemia, ↑ bilirubin, ↑ ammonia, renal dysfunction | Immediate delivery, ICU support, lactate‑free fluids |
| Viral Hepatitis (e.g., Hepatitis E) | Any trimester | Very high ALT/AST (>10× ULN), anti‑HEV IgM positive | Supportive care, consider ribavirin (post‑delivery) |
| Drug‑Induced Liver Injury | Variable | History of recent medication (e.g., acetaminophen >4 g/day), eosinophilia | Discontinue offending agent, N‑acetylcysteine if acetaminophen |
These four entities make up roughly 80 % of pregnancy‑related liver failures. Recognising the pattern early can shave days off a diagnostic odyssey.
Risk Factors & Potential Complications
Even when the trigger is treatable, several maternal and fetal risk factors magnify the danger:
- Multiparity - women with multiple prior pregnancies have a higher HELLP incidence.
- Pre‑eclampsia history - overlapping pathophysiology with HELLP and AFLP.
- Obesity and metabolic syndrome - predispose to fatty liver and drug‑induced toxicity.
Complications can be severe:
- Maternal mortality up to 15 % in AFLP, 8 % in severe HELLP.
- Fetal outcomes range from preterm birth to intra‑uterine death, especially if delivery is delayed.
- Long‑term sequelae such as chronic renal insufficiency or persistent coagulopathy.
Diagnosing Liver Failure Quickly
Time is the enemy. A practical diagnostic algorithm looks like this:
- Clinical suspicion: New jaundice, right‑upper‑quadrant pain, or altered mental status in any trimester.
- Basic labs: CBC, LFTs, INR, serum ammonia, blood glucose.
- Screen for specific causes:
- HELLP - check platelet count, LDH, uric acid.
- AFLP - use the Swansea criteria (≥6 of 14 findings, e.g., hypoglycemia, hyperuricemia).
- Viral serologies - Hepatitis A, B, E IgM/IgG.
- Medication review - focus on acetaminophen, antitubercular drugs, herbal supplements.
- Imaging: Ultrasound to rule out biliary obstruction; Doppler to assess hepatic blood flow if needed.
- Advanced testing (if diagnosis remains unclear): Transjugular liver biopsy - safe in coagulopathic patients.
Documenting the exact pattern of labs helps the multidisciplinary team pinpoint the cause and tailor therapy.

Treatment Options and Management Strategies
Therapy splits into two parallel tracks: stabilising the mother and optimising fetal outcome. Below is a step‑by‑step approach.
1. General Supportive Care
- ICU admission for continuous monitoring.
- Correct hypoglycemia with dextrose infusions.
- Maintain euvolemia; avoid fluid overload that worsens hepatic edema.
- Treat coagulopathy with fresh frozen plasma and vitamin K, but reserve blood products for active bleeding.
2. Cause‑Specific Interventions
- HELLP: Administer dexamethasone 10 mg IV every 12 h for 48 h to improve platelet counts, then plan delivery - usually by induction or Caesarean if fetal distress.
- AFLP: Prompt delivery is the only curative step; support with lactate‑free crystalloids, renal replacement therapy if needed, and monitor for hypoglycemia.
- Viral Hepatitis E: Mostly supportive; avoid hepatotoxic drugs. In severe cases after delivery, ribavirin may be considered under specialist guidance.
- Drug‑Induced: Stop the offending agent. For acetaminophen overdose, give N‑acetylcysteine within 8 h; continue for 24‑48 h if liver enzymes stay high.
3. Timing of Delivery
Delivery timing hinges on gestational age, maternal stability, and fetal status. General rules:
- If >34 weeks and maternal condition is deteriorating - proceed with delivery.
- If <34 weeks but mother is stable, consider corticosteroids for fetal lung maturity and monitor closely.
- In cases of severe encephalopathy or uncontrolled coagulopathy, earlier delivery may save the mother even at the cost of prematurity.
4. Post‑Delivery Follow‑Up
After birth, most liver function abnormalities resolve within 1‑2 weeks if the underlying cause was pregnancy‑specific. However, schedule:
- Liver panel at 1 week, 2 weeks, and 6 weeks.
- Renal function and coagulation profile until they normalise.
- Genetic counselling for families with recurrent AFLP (mitochondrial DNA mutations).
Management Checklist for Clinicians
- Recognise red‑flag symptoms: sudden jaundice, right‑upper‑quadrant pain, altered mental status.
- Obtain STAT labs: CBC, LFTs, INR, ammonia, glucose.
- Rule in/out specific causes using platelet count, LDH, renal function, viral serology, medication history.
- Transfer to ICU; start IV dextrose, correct electrolytes, give vitamin K.
- If HELLP suspected, give dexamethasone and plan delivery within 48 h.
- If AFLP suspected, organise delivery ASAP; prep neonatal team for preterm infant.
- Administer disease‑specific antidotes (e.g., N‑acetylcysteine for acetaminophen).
- Monitor fetal heart rate continuously; consider emergency Caesarean if distress.
- Post‑delivery, follow liver labs until normal; counsel on future pregnancy risks.
Frequently Asked Questions
Can liver failure in pregnancy be prevented?
Pre‑eclampsia screening, avoiding high‑dose acetaminophen, and managing metabolic syndrome reduce the odds of pregnancy‑related liver crises, but not all cases are preventable.
Is a C‑section always required?
No. Vaginal delivery is possible if the mother stabilises and there’s no immediate fetal distress. However, many severe cases prompt an urgent Caesarean for rapid delivery.
What is the prognosis for the baby?
If delivery occurs before severe maternal deterioration, neonatal survival exceeds 90 %. Prematurity remains the biggest risk when delivery happens early.
How long does liver recovery take after delivery?
In most HELLP or AFLP cases, liver enzymes and bilirubin normalize within 7‑14 days. Persistent abnormalities warrant further evaluation for underlying chronic disease.
Should women with a prior episode avoid future pregnancies?
Not automatically. With thorough pre‑conception counselling, close monitoring, and management of risk factors, many women have safe subsequent pregnancies.
By staying alert to the warning signs, ordering the right labs, and acting fast, clinicians can turn a frightening scenario into a manageable one. Early multidisciplinary care-obstetrics, hepatology, neonatology, and intensive‑care teams-remains the cornerstone of saving both mother and baby.


Eli Soler Caralt
October 21, 2025 AT 14:11One might muse that the liver, that silent alchemist of our bodies, chooses the most dramatic stage-pregnancy-to reveal its frailty, a reminder that even the most vital organ can be humbled by the miracle of life 😏. The cascade of HELLP and AFLP feels almost mythic, like a tragic hero stumbling in the labyrinth of hormones. Yet, the clinical reality is stark: early detection is the only savior, and that requires a vigilant eye and a willing heart. Definately, the balance between maternal and fetal safety is a philosophical tightrope.
Eryn Wells
October 22, 2025 AT 10:00Hey folks, just wanted to shout out how crucial it is to keep every pregnant patient’s community informed-no one should feel alone navigating liver failure. Sharing the checklist and the Swansea criteria in plain language can empower families worldwide 🌍. Let’s keep the conversation inclusive and make sure resources reach every corner, from city hospitals to remote clinics. Together we’re stronger! 😊
Kathrynne Krause
October 23, 2025 AT 06:50Wow, this whole breakdown is like a fireworks show of medical insight! 🎆 From the gritty details of platelet counts to the heroic rush of delivery, it’s a roller‑coaster of science and compassion. Remember, every data point is a brushstroke painting the picture of both mother and baby’s future. Stay fierce, stay informed, and let’s keep lighting up the darkness with knowledge! 💪
Chirag Muthoo
October 24, 2025 AT 03:40It is imperative, in the most solemn of terms, to recognise that timely delivery may constitute the singular curative intervention for acute fatty liver of pregnancy. By maintaining euvolemia and ensuring meticulous monitoring, clinicians can mitigate the risk of maternal demise. The synergy between obstetrics and hepatology must be orchestrated with precision. I remain optimistic that adherence to these protocols will continue to improve outcomes.
Angela Koulouris
October 25, 2025 AT 00:30Think of this as a training ground: every lab result, every vitals check is a step toward mastering the art of peripartum care. When you see elevated LDH, remember it’s not just a number-it’s a signal to act decisively. Keep your head high, trust your instincts, and let the interdisciplinary team be your safety net.
Harry Bhullar
October 25, 2025 AT 21:20The management of pregnancy‑related acute liver failure demands a multilayered approach that intertwines obstetric timing, hepatic support, and meticulous monitoring, each component being as critical as the next. First, early identification hinges on a high index of suspicion; clinicians should be alert to any new onset jaundice, unexplained encephalopathy, or coagulopathy irrespective of gestational age. Laboratory surveillance, including serial measurements of bilirubin, INR, and aminotransferases, establishes the trajectory of hepatic dysfunction and guides escalation of care.
Second, the decision matrix for delivery is nuanced. In cases where gestational age exceeds 34 weeks and maternal parameters are deteriorating, prompt induction or cesarean section is warranted to remove the fetal‑placental unit, which often acts as a persistent source of inflammatory mediators. Conversely, when pre‑viable, maternal stabilization via intensive‑care interventions-such as plasma exchange, renal replacement therapy, and controlled glucose infusion-takes precedence while fetal viability is closely reassessed.
Third, condition‑specific therapies must be instituted without delay. In HELLP syndrome, corticosteroids (dexamethasone 10 mg IV q12h) have shown benefit in improving platelet counts and reducing hepatic inflammation. For acute fatty liver of pregnancy, supportive care with lactate‑free crystalloids, early correction of hypoglycemia, and avoidance of hepatotoxic drugs are paramount; liver transplantation remains a last resort but has been successfully employed in refractory cases.
Fourth, the multidisciplinary team should operate under a shared checklist. This includes confirming blood product availability, arranging for neonatal intensive‑care standby, and documenting all therapeutic interventions in real time. Communication channels between obstetrics, hepatology, anesthesiology, and neonatology must be fluid, minimizing any lag that could jeopardize outcomes.
Finally, post‑delivery monitoring is essential because hepatic recovery may lag behind obstetric resolution. Serial imaging to assess hepatic perfusion, continued assessment of coagulation status, and evaluation for secondary complications such as infections or renal insufficiency are vital. In summary, the orchestration of rapid diagnosis, timely delivery, targeted therapy, and coordinated team dynamics forms the cornerstone of improving survival for both mother and child in the setting of pregnancy‑associated liver failure.
Dana Yonce
October 26, 2025 AT 17:10Totally blew my mind seeing how a simple acetaminophen overdose can trigger such chaos, especially when the dosage creeps over the 4 g/day line 🚨. It’s a stark reminder to double‑check med charts, even for “harmless” drugs.
Lolita Gaela
October 27, 2025 AT 14:00From a hepatopathological perspective, the perturbation of the hepatic microvascular architecture in HELLP precipitates a cascade of endothelial dysfunction, culminating in platelet sequestration and fibrin deposition. This pathophysiological milieu underscores the necessity for high‑dose corticosteroid regimens to attenuate the cytokine surge. Moreover, the utilization of N‑acetylcysteine in non‑acetaminophen–induced ALF serves as a glutathione precursor, ameliorating oxidative stress within hepatocytes.
Giusto Madison
October 28, 2025 AT 10:50Yo, if you think you can just ignore the Swansea criteria and wing it, you’re asking for disaster-stop playing games with lives! The data is crystal clear: early delivery saves moms and babies, period.
erica fenty
October 29, 2025 AT 07:40Quick tip: monitor INR daily, act fast!!!
Xavier Lusky
October 30, 2025 AT 04:30The pharma giants love to hide the true danger of certain herbal supplements during pregnancy, steering us toward synthetic drugs that keep the profit wheels turning while the real risks are swept under the rug.
Ashok Kumar
October 31, 2025 AT 01:20Oh, sure, because juggling a liver transplant and a third trimester is just another Tuesday, right? Let’s all pretend it’s easy while the odds keep stacking against you.
Jasmina Redzepovic
October 31, 2025 AT 22:10Look, anyone who doubts the superiority of our national healthcare protocols clearly hasn’t read the latest WHO comparative analysis-our guidelines on managing AFLP are unmatched, and we set the global standard.
Esther Olabisi
November 1, 2025 AT 19:00Totally agree that every system has its shine, but maybe we could all benefit from a little cross‑border knowledge sharing-after all, even the best can learn a trick or two from a neighbor 🌏😊.
Rachel Valderrama
November 2, 2025 AT 15:50Well, if we all just followed the checklist like obedient robots, maybe the whole “miracle of life” thing wouldn’t feel like a high‑stakes drama every single time 🙄.