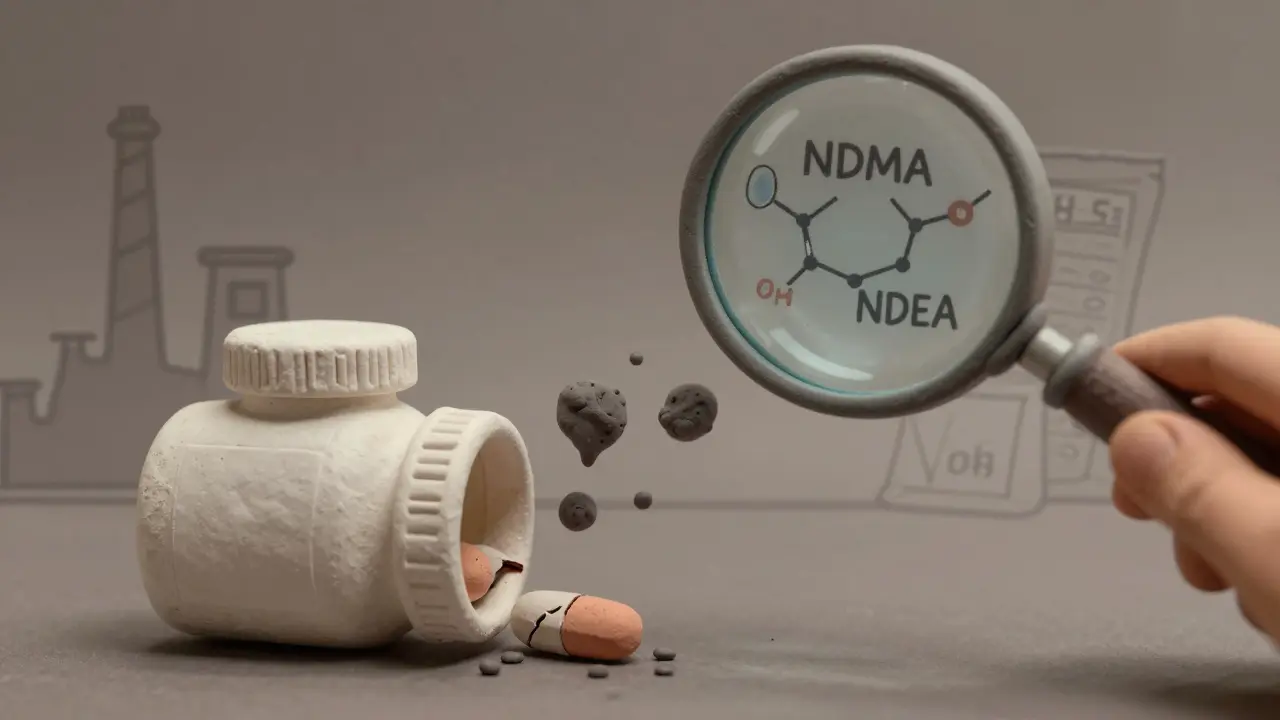
Back in 2018, a routine test on a batch of generic blood pressure medicine turned up something terrifying: a chemical linked to cancer. It wasn’t a rare lab error. It was a pattern. That chemical was nitrosamine-specifically NDMA-and it showed up in valsartan, a common generic drug. What followed wasn’t just a recall. It was a slow-burning crisis that shook the entire generic drug industry and forced regulators, manufacturers, and patients to rethink what ‘safe’ really means.
How Did Nitrosamines End Up in Our Medicine?
Nitrosamines aren’t added on purpose. They’re accidental byproducts. They form when certain chemicals in the manufacturing process react under heat, pressure, or storage conditions. Think of it like rust on a car-but inside your pill. The main culprits? Secondary amines (common in drug ingredients) meeting nitrites (often hiding in excipients like magnesium stearate or even packaging materials). It took years for scientists to catch on. For decades, manufacturers focused on making sure the active ingredient was pure. They didn’t test for trace impurities at the parts-per-billion level. But nitrosamines don’t need much to be dangerous. The FDA says even 96 nanograms per day of NDMA over a lifetime could raise cancer risk. That’s less than a grain of salt in a swimming pool. The first big wave hit in 2018 with ARBs-drugs like valsartan, losartan, and irbesartan. Then came ranitidine (Zantac), metformin for diabetes, duloxetine for depression, and even varenicline for smoking cessation. By mid-2025, over 500 drug products had been recalled globally because of nitrosamine levels. Some batches contained over 1,500 ng/day-15 times the safe limit.Who’s Being Affected-and How Bad Is It?
The impact isn’t just numbers. Real people stopped taking their meds. Some switched to brand-name versions, which cost 10 to 20 times more. Others went without, risking uncontrolled high blood pressure or diabetes. Hospitals saw spikes in emergency visits from patients who skipped doses out of fear. The FDA confirmed that the contamination wasn’t limited to one factory or one country. It was systemic. Manufacturers in India, China, and Europe-all using similar processes-were affected. One case study showed a simple change in the supplier of magnesium stearate led to NDEA formation in three different ARB products. That’s not a fluke. It’s a design flaw buried in the supply chain. Even packaging played a role. Blister packs and bottle liners made with amine-based adhesives started showing up as nitrosamine sources in 2022. A generic antibiotic tablet recall in 2024 traced contamination to the adhesive in the foil backing. No one had tested that before.The FDA’s Response: Fast, But Overwhelming
The FDA moved quickly. In 2019, they published initial limits for NDMA and NDEA. By 2023, they released a detailed guide for nitrosamine drug substance-related impurities (NDSRIs)-compounds unique to each drug. For example, N-nitroso-varenicline has a limit of 96 ng/day, while NDEA is capped at 26.5 ng/day. But here’s the catch: if a drug has more than one nitrosamine, the limits don’t just add up-they multiply risk. Two impurities at 80% of their individual limits? That’s 160% of safe exposure. The FDA didn’t just ask companies to test. They demanded root cause analysis, reformulation, and stability data proving the fix lasts through the product’s shelf life. The cost? For a mid-sized generic maker, it’s $500,000 to $2 million per year just to test and rework one line. One company spent 18 months and $2 million fixing their metformin production. Another spent 14 months switching suppliers after a single bad batch of excipient ruined three products.
Global Differences: Who’s Doing It Right?
The U.S. didn’t go it alone. The European Medicines Agency (EMA) issued 32 recalls. Health Canada, the UK’s MHRA, and Japan’s PMDA each had 5-15. But the FDA’s rules are stricter. The EMA allows broader, generic limits for some impurities. The FDA requires compound-specific limits. That’s more accurate-but harder to execute. Small manufacturers in emerging markets struggled. Many didn’t have the lab equipment to detect nitrosamines at 0.3 ng/mL. Some didn’t even know where to start. In June 2025, the FDA made a major shift. They pushed back the August 1, 2025 deadline for full NDSRI compliance. Now, manufacturers just need to submit progress reports. It’s not a waiver-it’s a recognition that fixing this isn’t like flipping a switch. It’s a multi-year engineering project.Who’s Surviving-and Who’s Getting Left Behind?
The crisis has reshaped the generic drug market. Smaller companies are disappearing. One manufacturer in Florida shut down after failing to pass three consecutive nitrosamine audits. Another in India lost its FDA approval after a single batch of varenicline came back contaminated. The winners? Big players with deep pockets and strong quality systems: Teva, Fresenius Kabi, Sun Pharma. They invested early. They built in-house labs. They redesigned processes before they were forced to. Sun Pharma recalled a Vyvanse generic in late 2025-but they did it proactively. That earned them trust from regulators. Now, the FDA gives faster review to companies with proven nitrosamine controls. It’s not just about safety anymore. It’s about competitiveness.