Every time you or someone you care about takes a prescription drug, there’s a hidden document behind it - one that holds everything you need to know about safety, risks, and how to use it correctly. It’s not the bottle label. It’s not the patient leaflet. It’s the FDA drug label, also called the Full Prescribing Information (FPI). And if you don’t know how to read it, you’re missing critical details that could affect your health.
What Exactly Is the FDA Drug Label?
The FDA drug label isn’t something you find on the pharmacy shelf. It’s the official, legally required document that tells doctors, pharmacists, and regulators everything about a drug - from how it works to what can go wrong. This isn’t marketing material. It’s a technical, science-based summary approved by the U.S. Food and Drug Administration and updated regularly. Every prescription drug sold in the U.S. must follow this exact format, which was standardized in 2006 and refined through 2024.
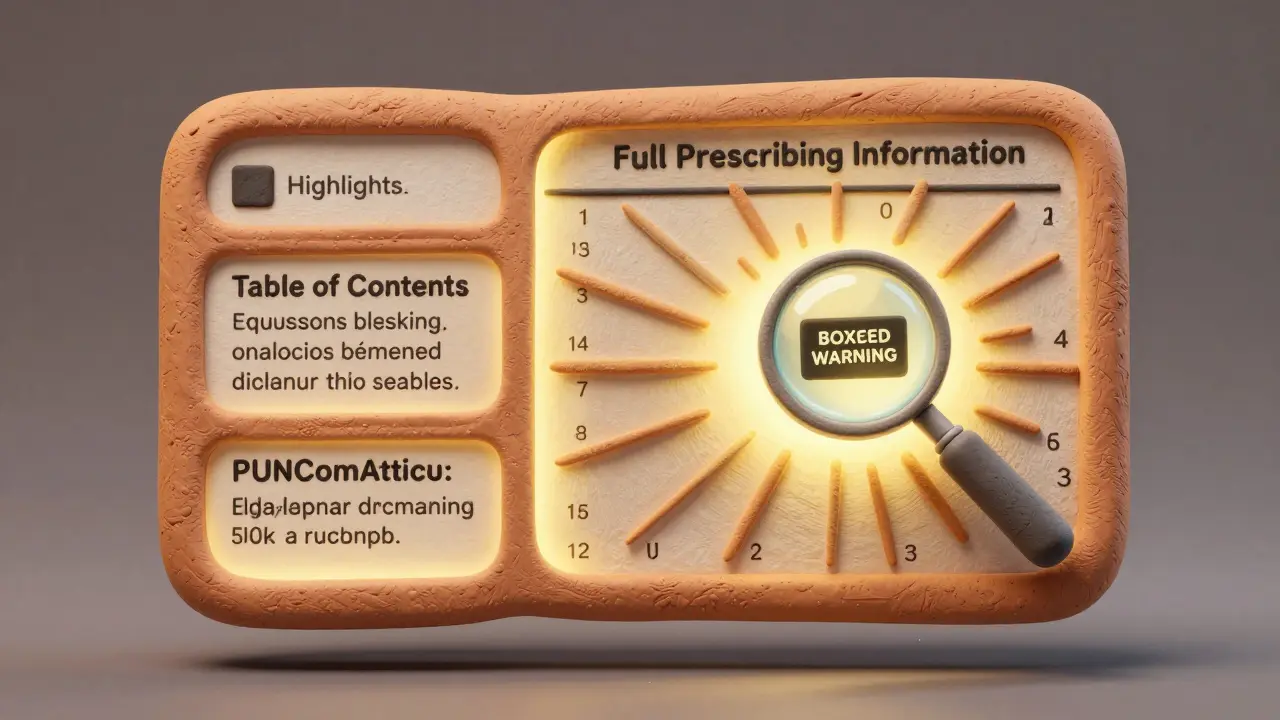
It’s divided into three main parts: the Highlights, the Table of Contents, and the Full Prescribing Information. The Highlights are just a quick snapshot - half a page max - and they’re designed to catch your attention. But here’s the catch: they’re incomplete. The FDA requires them to say so right on the page. If you stop reading after the Highlights, you’re missing up to 90% of the important details.
The 17 Sections of the Full Prescribing Information
The real meat of the label is in the Full Prescribing Information. It’s broken into 17 numbered sections. Each one has a specific purpose, and knowing where to look saves time - and maybe your life.
- Section 1: Indications and Usage - This tells you exactly what the drug is approved to treat. Don’t assume it works for anything off-label unless your doctor says so. This section also includes the drug’s Established Pharmacologic Class (EPC), like “beta-blocker” or “SGLT2 inhibitor,” which helps you understand how it works in the body.
- Section 2: Dosage and Administration - This is where you find the right dose, how often to take it, and how to adjust it for kidney or liver problems. The 2024 FDA update made this section clearer about dose changes for older adults and people with organ impairment. Missing this can lead to underdosing or dangerous overdosing.
- Section 3: Dosage Forms and Strengths - Lists every version of the drug: tablets, capsules, injections, etc., and their strengths (like 10 mg, 25 mg). This helps you spot look-alike drugs - a common cause of pharmacy errors.
- Section 4: Contraindications - These are the “DO NOT USE” situations. If you have a known allergy, certain heart conditions, or are pregnant and the drug is labeled unsafe, this section says so plainly.
- Section 5: Warnings and Precautions - This is the most critical section after the Boxed Warning. It includes everything from liver damage risks to psychiatric side effects. The Boxed Warning - a black border around the most serious risks - appears at the very top of this section. If you see it, stop and read it twice.
- Section 6: Adverse Reactions - Lists side effects from clinical trials, with percentages showing how often they happened. If something happens in 5% or more of patients, it’s listed. But remember: real-world side effects can be more common than trial data shows.
- Section 7: Drug Interactions - This tells you what other drugs, foods, or supplements could make this one dangerous. For example, some statins can’t be taken with grapefruit juice. Others interact with blood thinners. Skipping this can lead to hospitalization.
- Section 8: Use in Specific Populations - Covers pregnancy, breastfeeding, children, and elderly patients. Many drugs are not tested in pregnant women, so this section often says “data not available.” That doesn’t mean it’s safe - it means it’s unknown.
- Section 9: Drug Abuse and Dependence - For controlled substances like opioids or stimulants, this section explains addiction risk, withdrawal symptoms, and abuse potential.
- Section 10: Overdosage - What happens if someone takes too much? Symptoms, treatment options, and whether dialysis helps. This is rarely read - but it’s lifesaving in emergencies.
- Section 11: Description - The chemical name and structure. Mostly for experts, but if you’re curious, this is where you find it.
- Section 12: Clinical Pharmacology - How the drug moves through the body: absorption, metabolism, half-life. Useful if you’re wondering why you take it at night or with food.
- Section 13: Nonclinical Toxicology - Animal study data on cancer risk, gene mutations, and long-term toxicity. Rarely reviewed by patients, but important for long-term use decisions.
- Section 14: Clinical Studies - Summaries of the trials that proved the drug works. This is where you see if it was tested on people like you - older adults, people with diabetes, etc.
- Section 15: References - Links to the scientific papers behind the claims. Not always useful for patients, but gold for clinicians.
- Section 16: How Supplied/Storage and Handling - Lists the National Drug Code (NDC), a 10-digit number that identifies the exact product, manufacturer, and package size. Also tells you how to store it - refrigerate? Keep away from light? This matters for effectiveness.
- Section 17: Patient Counseling Information - The FDA’s suggested talking points for doctors to share with patients. Things like “Don’t stop this suddenly,” or “This may make you dizzy.” Yet, only about 38% of providers actually use this section during consultations.
What Is the Boxed Warning?
Think of the Boxed Warning as the FDA’s red alarm. It’s the most serious risk the drug carries - things like sudden death, severe liver failure, or suicidal thoughts. It’s not buried. It’s at the top of Section 5, surrounded by a thick black border. If you’re prescribed a drug with a Boxed Warning, ask your doctor: “Why is this risk worth taking?” And make sure you understand what symptoms to watch for.
For example, some antidepressants carry a Boxed Warning for increased suicide risk in young adults under 25. That doesn’t mean you shouldn’t take them - but you need to know the signs and have a plan.

What Is the “Recent Major Changes” Section?
Since 2018, every FDA label must include a section that lists what changed in the last six months. This could be a new warning, updated dosage, or a removed contraindication. If your doctor prescribed this drug a year ago, the label might have changed. Always check this section before refilling - especially if you’ve had a new side effect or started another medication.
Studies show that when doctors review this section, they catch safety updates 35% faster. That’s not just efficiency - it’s risk reduction.
How Do Healthcare Providers Actually Use This?
Doctors don’t read the whole thing every time. They follow a smart shortcut:
- First: Look at the Boxed Warning and Highlights. What’s the biggest danger?
- Second: Check Section 1 (Indications) - Is this the right drug for the condition?
- Third: Go to Section 2 (Dosage) and Section 7 (Interactions) - Is the dose right? What else is the patient taking?
- Fourth: If something’s off - like kidney issues or pregnancy - check Section 8.
Pharmacists focus on Section 2 (dosing), Section 3 (formulations), Section 6 (side effects), and Section 16 (NDC code). That’s because 12.7% of dispensing errors come from confusing similar-looking drugs - and the NDC helps avoid that.
What About Patients? Can You Read It Too?
Yes - and you should. The FDA’s Patient Counseling Information (Section 17) is written for you. It’s plain language. It tells you what to watch for, what to avoid, and what to tell your doctor.
But here’s the problem: most patients never see it. A 2024 study found that 27% of people rely only on the Highlights section - and miss the serious risks. One woman took a blood thinner because she saw it was “for preventing clots.” She didn’t know it could cause bleeding in the brain. That warning was in Section 5 - not in the Highlights.
If you’re prescribed a new drug, ask for the Full Prescribing Information. You can find it on the FDA’s website or ask your pharmacist for a printed copy. Don’t settle for the bottle label. That’s just a summary.
What’s Changing in 2025 and Beyond?
The FDA is working on something called the “Patient-Focused Labeling Initiative.” That means future labels might include simpler summaries, icons for risks, or even QR codes that link to video explanations. The goal? Make it easier for patients to understand without losing the detail doctors need.
Right now, 98% of electronic health records pull drug info directly from the FDA’s Structured Product Labeling (SPL) system - an XML-based format that computers can read. That’s why your app or online portal shows accurate drug info. Behind the scenes, it’s all coming from this label.
By 2027, many new drugs may come with interactive digital labels. You’ll be able to click “Show me side effects for seniors” or “What happens if I miss a dose?” - all based on the same official data.
What Happens If the Label Is Wrong?
It’s illegal. The FDA can issue warning letters, force recalls, or even ban a drug. In 2023 alone, 47 companies got warning letters for labeling errors - like missing warnings, incorrect dosing, or wrong NDC codes.
That’s why the label is so tightly controlled. Every word is reviewed by FDA scientists. Every number is verified. It’s not perfect - but it’s the most reliable source you have.
Bottom Line: What You Need to Do
Here’s your action plan:
- Always ask for the Full Prescribing Information - not just the patient leaflet.
- Check the Boxed Warning first. If there’s one, understand it.
- Look at Section 2: Is the dose right for you? (Age, weight, kidney function?)
- Check Section 7: Are you taking anything else that could interact?
- Read Section 17: It’s written for you - and it’s the only part designed to help you stay safe.
- Recheck the “Recent Major Changes” section every time you refill.
Drug labels aren’t meant to be scary. They’re meant to be clear. And when you know how to read them, you’re not just following instructions - you’re taking control of your health.

Mindee Coulter
January 29, 2026 AT 06:31Finally someone explains this without fluff. I work in pharma and even I skip to Section 2 and 7 most days. The rest is noise unless something goes wrong.
Colin Pierce
January 29, 2026 AT 07:14This is gold. I print out Section 17 for every new patient. Most don’t know it exists. Last week a guy came back because he thought his blood pressure med was supposed to make him dizzy - turned out he skipped the ‘may cause orthostatic hypotension’ line. Simple fix.
Anna Lou Chen
January 30, 2026 AT 05:56Let’s be real - the FDA label is a bureaucratic monument to liability, not patient empowerment. It’s written in legalese disguised as science, optimized for lawyers, not lives. The ‘Patient Counseling Information’? A performative gesture. No one reads it. No one *can* read it. It’s designed to make regulators feel safe while patients drown in jargon. The real problem isn’t the label - it’s the system that treats human beings like data points.
Section 12? Clinical pharmacology? Who the hell is supposed to parse half-life kinetics before taking a pill? You’re telling me a 72-year-old with diabetes and three prescriptions is going to decode CYP450 interactions? This isn’t transparency - it’s therapeutic overkill.
The Boxed Warning? Sure, it’s dramatic. But it’s also the only part that matters. Everything else is noise engineered to distract from the fact that 80% of these drugs have marginal benefit. We’ve turned pharmacology into a spectator sport where patients are the audience, not the actors.
And don’t get me started on the ‘Recent Major Changes’ section. It’s buried. No one checks it. The FDA updates it like it’s a Wikipedia edit. Meanwhile, people are dying because a new drug interaction popped up in June and their doctor hasn’t opened the label since 2021.
QR codes? Interactive labels? Cute. But if you can’t get a pharmacist to explain Section 6 without reading it verbatim, then digital glitter won’t save you. The problem isn’t format - it’s access. And trust. And the fact that we’ve outsourced health literacy to corporations who profit when you don’t understand what you’re taking.
Until we stop treating medication like a black box and start treating patients like people who deserve to know what’s in it - all the labeling in the world is just theater.
And yes, I’ve read the entire label. Twice. And I still feel like I’m being gaslit by a 300-page PDF.
Mark Alan
January 31, 2026 AT 06:10USA FOREVER 🇺🇸💪 The FDA gets it RIGHT. No other country has this level of transparency. Europe? They hide the bad stuff. China? They don’t even publish labels. This is AMERICAN excellence. If you don’t read the label, that’s YOUR fault. Not the FDA’s. 🚫💊
Ambrose Curtis
February 1, 2026 AT 15:28bro i just googled the drug name + side effects and it’s way easier than reading this whole thing. also why is section 13 even a thing? who cares about rat cancer studies? 🤡
but seriously - section 7 saved me. took a zpack and then had a beer. ended up in the ER. now i always check interactions. dumb but life-saving.
Linda O'neil
February 2, 2026 AT 14:53You’re not alone if this feels overwhelming. I used to panic every time I got a new script. Then I started keeping a little notebook - drug name, section 2 dose, section 7 interactions, section 17 warning. Now I feel like a superhero. You got this. One section at a time.
James Dwyer
February 3, 2026 AT 20:14There’s a quiet power in knowing what’s really in that pill. Not fear. Not confusion. Just clarity. That’s what this label gives you - if you’re willing to look.
jonathan soba
February 5, 2026 AT 05:28Interesting that you mention Section 14 - clinical studies. But you don’t address the elephant in the room: 73% of those trials are funded by the drug manufacturer. The data is cherry-picked. The ‘efficacy’ is statistically significant but clinically meaningless. You’re celebrating a marketing document dressed as science.
And the ‘Recent Major Changes’? That’s the FDA’s way of saying, ‘We caught another lie last month.’ It’s not a feature - it’s a failure.
Phil Davis
February 5, 2026 AT 11:50So you’re telling me I need to read 17 sections to take a pill… but my doctor doesn’t even know what’s in Section 8? 😅
Also, why is Section 11 called ‘Description’? That’s just the chemical formula. I didn’t sign up for organic chemistry.
Irebami Soyinka
February 5, 2026 AT 15:47USA be like: ‘Here’s 300 pages on your medicine!’ 🇺🇸 Nigeria be like: ‘Here’s one tablet. No label. Hope you live.’ 🇳🇬😂 We don’t need QR codes. We need *medicine*.
doug b
February 7, 2026 AT 02:43Just read section 2 and 7. That’s 90% of what you need. If your doctor’s prescribing something and won’t explain those two, find a new one. Simple.
Mel MJPS
February 7, 2026 AT 22:06My grandma didn’t read any of this. But she always asked, ‘Does this make you sleepy?’ and ‘Will it mess with my heart?’ That’s all that mattered. Sometimes the human questions are the right ones.
Katie Mccreary
February 8, 2026 AT 17:46Why do you think people don’t read it? Because they’ve been burned before. My last med gave me suicidal thoughts. The label said ‘rare.’ It happened to me. Now I don’t trust labels. I trust gut.
SRI GUNTORO
February 9, 2026 AT 05:38People today think they deserve to know everything. Back in my day, you took the pill and didn’t ask questions. Trust your doctor. That’s what faith means.
Kevin Kennett
February 10, 2026 AT 01:13Look - I’m a nurse. I’ve seen people die because they didn’t know a drug interacted with their grapefruit juice or their fish oil. This isn’t just info - it’s armor. Read Section 17. Say it out loud to your doctor. Make them confirm it. You’re not being difficult. You’re being smart.